“Virtual Coach” to monitor Powered Seat Functions (PSF) usage
Rosemarie Cooper MPT,ATP1,2 , Rory A Cooper, PhD1,2 , Jon Pearlman, PhD1,2 ,
Hsin-yi Liu, BS1,2, Asim Smailagic, PhD3
1 Human Engineering Research Laboratories, VA Pittsburgh Medical Center, Pittsburgh, PA;
2 Department of Rehabilitation Science and Technology, University of Pittsburgh, Pittsburgh, PA
3 Quality of Life Technology Center, Carnegie Mellon University, Pittsburgh PA
ABSTRACT
Insurers have questioned the value of powered seat functions (PSF) because some individuals who have been provided them still experience problems with pressure ulcers, spasticity or pain. Clinicians must currently prescribe electric power wheelchairs (EPW) and power seat functions based upon clinical examination and consumer interviews without community usage data. Little is known about the actual usage of these systems and its effectiveness. This paper will provide an overview of the work conducted in Pittsburgh on current data logging systems and introduce the novel approach of the “virtual coach” (VC) a programmable, intelligent reminder to provide guidance to encourage desired PSF usage and provide insightful community usage data. The “virtual coach” could improve compliance with clinician recommendations and reduce incidence of secondary conditions.
KEYWORDS
virtual coach, electric powered wheelchairs, powered seat functions, data-logging systems,
BACKGROUND:
High cost electric powered wheelchairs (EPW) offer powered seating functions (PSF) such as tilt-in-space, backrest recline, leg elevation, and seat elevation. A full complement of PSF can double the cost of an electric powered wheelchair, thus it is important to investigate the outcomes PSF can realistically deliver in community settings. Clinicians must currently prescribe EPW based upon clinical examination and consumer interviews without community usage data. Little is known about the actual usage of these systems. Insurers have questioned the value of PSF because some individuals who have been provided them still experience problems with pressure ulcers, spasticity or pain. It is as yet unknown whether these continuing problems are due to ineffective usage of the technology, whether the technology is insufficient, or whether other factors or combinations of factors are influencing the outcomes.[1]
The Consortium for Spinal Cord Injury Clinical Practice Guidelines (CSCI-CPG), (see www.pva.org), and the Rehabilitation Engineering and Assistive Technology Society of North America (RESNA) “Position Papers,” (see www.resna.org), recommend the use of tilt and recline systems for pressure management and seating elevation systems for preservation of upper limb function.[2] The recommendation on pressure management is based upon studies conducted in clinical or laboratory settings and focus on blood flow, blood profusion, and surface pressure, with the vast majority of the studies relying solely on surface pressure readings. Medicare and some private payers do not cover power seat elevators. The clinical literature indicates that 40 or more degrees of tilt and/or 120º or more of rearward backrest recline every fifteen minutes for two minutes or more are indicated.[3] Some clinicians and consumers believe that this is simply too onerous, and that “active seating” is adequate; “active seating” is defined as consumer initiated frequent position changes in various directions to differing degrees. Through data logging, the therapist could obtain a profile of the user’s seating activity to review before placing the final order. This paper will provide an overview of the work conducted in Pittsburgh on current data logging systems and introduce the novel approach of the “virtual coach” (VC) a programmable, intelligent reminder to provided guidance to encourage desired PSF usage and provide insightful community usage data.
DESCRIPTION:
Since the VC is based upon the integration of several of current data-logging systems developed here in Pittsburgh, we will provide a brief description of the work and studies conducted related to these systems.
Powered Seating Function Utilization Monitoring
We conducted a pilot PSF research study in 2006 in which a Seat Feature Data Logger (SFDL) was attached to 11 subject’s personal wheelchairs for 10-14 days to gather data regarding daily usage of the wheelchair and these features.[4] (see Table 2). Based on these data, subjects were found to spend significantly more time in a tilted versus an upright position (p<0.025), but tilt was not used significantly more than recline (p=0.155) or seat elevation (p=0.046). In addition, comparison of SFDL data with pressure-mapping data revealed that subjects were more likely to use small and intermediate amplitude tilt and recline angles, and positions known to result in low peak pressure were accessed more frequently and for longer durations than intermediate and high pressure positions. While subjects did not always use the angles of tilt and recline – as many clinicians recommend – these features were used frequently and their use resulted in associated lower peak pressures. Our preliminary data showed that there was a need for collecting more data (e.g., center of mass) more reliably, on a wider variety of EPW, and for longer periods of time.
Means |
|
|---|---|
| Duration EPW occupied | 12.0 ± 3.0 hours/ day |
| Transfers completed | 5.0 ± 5.3 per day |
| Duration backrest in upright position | 0.7 ± 1.5 hours/day |
| Tilt feature accessed | 18.4 ± 14.4 times/day for 8.5 ± 5.2 hours/day |
| Recline feature accessed | 11.5 ± 8.4 times/day for 8.6 ± 4.6 hours /day |
| Duration Tilt-&-Recline used in combination | 4.8 ± 4.6 hours/day |
| Seat-elevation accessed | 4.3 ± 4.1 times/day for 2.8 ± 4.6 hours day. |
Wheelchair Activity Monitoring
 Figure 1. Data loggers for Electric Power Wheelchairs (left) and Manual Wheelchairs (right) (Click for larger view)
Figure 1. Data loggers for Electric Power Wheelchairs (left) and Manual Wheelchairs (right) (Click for larger view) HERL has made important strides in the development of an EPW activity monitor, which is a cornerstone of a ‘research module’ for the NIDRR Spinal Cord Injury Model Systems.[5] This device was used on both power and manual wheelchairs in a study by Cooper et al (2002), (Figure 1).[6] In a more recent study, improvements were made to a Caster Data Logger (CDL) for EPW and were used to collect pilot EPW usage data during and after the National Veterans’ Wheelchair Games (NVWG). Subjects who used an EPW as their primary means of mobility were recruited at the NVWG for this study. In five days at the games, the participants (n=5) traveled a distance of 7751 ± 3439m per day, while traveling 3397±1300 m (n = 4) per day during five days of the following week. The CDLs performed well and should become a valuable usage measuring tool.
Vibration Data-Logger
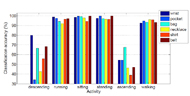 Figure 2. Recognition accuracy for typical activities at several body locations (Click for larger view)
Figure 2. Recognition accuracy for typical activities at several body locations (Click for larger view) A vibration data logger was developed at HERL by adopting a low-power microcontroller (MSP430F149) from Texas Instruments Inc. that was used in the wheel rotation data logger, and replaced the flash memory with a Secure Digital (SD) card for larger capacity. The microcontroller, SD card, and a MEMS dual-axis accelerometer were held in a small self-contained rectangular box, which was readily attached underneath the seat pan. This data logger hasn’t been used in any field studies yet, however, we used the same type of accelerometer placed underneath the seat and connected with a laptop to measure vibration exposure during wheelchair propulsion.[7] In this project, instead of focusing on vibration, we will examine the acceleration for determining the type activity (e.g., riding in a car) for the virtual coach.
eWatch
The Virtual Coach is built upon our previous custom data logging work as well as that on the eWatch, developed by researchers at Carnegie Mellon University , which is a wearable sensor and notification platform developed for context aware computing research.[8][9] It fits into a wrist watch making it instantly viewable and socially acceptable (see Figure 3). The eWatch architecture consists of a main CPU, sensors, power control, notification mechanisms, and wireless communication. eWatch is capable of sensing temperature, light, two axes of acceleration and audio input at user controllable sampling rate up to 100KHz. The user can be notified of an event or desired activity using a 128x64 pixel display, an LED, vibrating motor and tone generating buzzer. Three push buttons are distributed around the outside of the housing in the standard configuration of a digital watch. 18 The eWatch platform has been used to identify previously visited locations. Data were recorded from the light and audio sensors at several different locations including the user’s apartment, office, lab, street locations, interior of a bus, restaurant and supermarket. Prior experiments also demonstrated the versatility of using e-Watch located in various body positions for detecting a wide range of activities such as standing, sitting, walking, running, ascending stairs, and descending stairs.
Virtual Coach
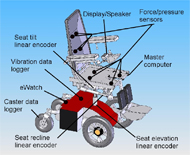 Figure 4. SolidWorks drawing of the virtual coach with partial list of sensors shown. (Click for larger view)
Figure 4. SolidWorks drawing of the virtual coach with partial list of sensors shown. (Click for larger view) The virtual coach (VC) is a portable, programmable intelligent reminder. Unlike a simple “scheduler” time reminder with limited utility, the VC will not be based upon time; rather, it uses artificial intelligence techniques to provide guidance to encourage the desired behavior. For example, a timer based system may indicate that a person should tilt his seat for 2 minutes at 9:00 am. However, these systems currently do not know that the person may have tilted his or her seat from 8:50 to 8:52 am, and therefore the user may become annoyed by the reminder. Standard reminder systems also do not know if the person tilted or reclined far enough, whereas the virtual coach can encourage people to tilt/recline a bit more or for a while longer. The coach will include sensing, logging, and modeling. The modeling ranges from statistical to inferential. The VC will also be able to infer activity, for example driving, and postpone the reminder or alter the reminder if in a movie theater. The VC will monitor user performance in compliance with clinician practice guidelines for usage of their seating functions and provide appropriate feedback and encouragement. As the user’s compliance changes, the coach may reduce the number of verbal cues as the subject learns or provide increased support as needed. The virtual coach will also provide constant and consistent observation/monitoring, even on a real-time basis, thereby extending the clinician’s guidance beyond episodic patient examinations. Machine learning will be utilized to adapt as an individual’s situations and compliance with guidelines change. Elements of game design will be utilized to keep the users engaged.
DISCUSSION:
Of course, what is ultimately needed is a training program (which will likely require further refinement based upon what is learned in a study) that is proven to be effective and clinically practical (with a Medicare code for wheelchair training, this is more attractive) combined with a long-term clinical trial to actually demonstrate that the occurrence of pressure ulcers is reduced. Manufacturers currently provide no clinician accessible recording devices on EPW. Reliable activity data can enhance quality assurance and warranties, improve clinical decision making and support evidence based medicine. Activity instrumentation built-in at the factory would have little effect on the total EPW cost.
CONCLUSION:
The “virtual coach” could improve compliance with clinician recommendations and reduce incidence of secondary conditions and should reduce the barriers of current modes of service and support delivery and assuring safety.
REFERENCES:
- Lacoste M, Weiss-Lambrou R, Allard M, Dansereau J. Powered tilt/recline systems: why and how are they used? Assist Technol. 2003;15:58-68.
- Paralyzed Veterans of America. Pressure ulcer prevention and treatment following spinal cord injury: A clinical practice guideline for healthcare professionals. Accessed on 2-14-2007 at URL: http://www.guidelines.gov/summary/summary.aspx?doc_id=2589&nbr=001815& string=%22decubitus+ulcers%22+AND+sci . Last Updated: 8-4-2000.
- Hobson DA. Comparative effects of posture on pressure and shear at the body-seat interface. J Rehabil Res Dev. 1992;29:21-31.
- Leister, E. P. The effectiveness and use of seat tilt, backrest recline, and seat elevation in adult powered wheelchair users. Master's Thesis. 2006. University of Pittsburgh.
- Spaeth, D. M., Arva, J., and Cooper, R. A. Application of a Commercial Datalogger for Rehabilitation Research. Proceedings of the 23rd Annual Rehabilitation Engineering & Assistive Technology Conference, 381-383. 2000. 6-15-2000.
- Cooper RA, Thorman T, et al. Driving characteristics of EPW users: how far, fast, and often do people drive? Arch Phys Med Rehabil. 2002;83:250-255.
- Burns SP, Betz KL. Seating pressures with conventional and dynamic wheelchair cushions in tetraplegia. Arch Phys Med Rehabil. 1999;80:566-571.
- VanSickle DP, Cooper RA, Boninger ML, DiGiovine CP. Analysis of vibrations induced during wheelchair propulsion. J Rehabil Res Dev. 2001;38:409-421.
- Maurer, U., Smailagic, A., Siewiorek, D., and Deisher, M. Activity recognition and monitoring using multiple sensors on different body positions. 113-116. 2006. IEEE International Workshop on Wearable and Implantable Body Sensor Networks. 2006.
- Maurer, U., Rowe, A., Smailagic, A., and Siewiorek, D. eWatch: A wearable sensor and notification platform. IEEE International Workshop on Wearable and Implantable Body Sensor Networks[2006]. 2006.
Author Contact Information:
Rosemarie Cooper, MPT,ATP, University of Pittsburgh -Center for Assistive Technology, Forbes Tower, Suite 3010, 3600 Forbes Avenue at Atwood, Pittsburgh, PA 15213
Office Phone (412) 647-1315, EMAIL: cooperrm@pitt.edu
